What is COVID-19?
COVID-19 is a disease caused by a virus that mostly affects the respiratory tract (that’s the lungs and airways, to you and me), and is thought to have originated in China. A virus consists of genetic material surrounded by a protein and sometimes a lipid coat. Viruses themselves cannot survive or replicate without invading the the cells of living organisms, and for this reason they are widely considered not to be “alive” in the traditional sense. Viruses are different from bacteria – for example bacteria are living organisms that can exist independently of other forms of life – which is why antibiotics, which act against bacteria, do not work on viruses.
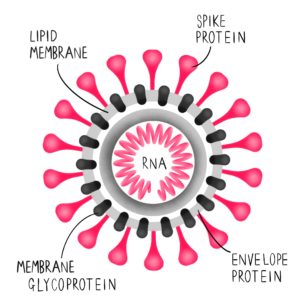
More specifically, the virus that causes COVID-19 is a specific type of virus called a coronavirus. Coronaviruses are so named because their virions (that’s the protein on the outer layer of the virus, which is the infective part of the virus) have a distinctive crown-like appearance. The Latin word for crown is “corona.”
There are many coronaviruses, the majority of which cause mild cold or flu symptoms and pose no major threat to humans. But there are three coronaviruses that do pose a risk to humans, as they can cause severe respiratory failure or death, even in healthy young people. These three coronaviruses are called:
- SARS-CoV. This is the virus that was responsible for the 2003 Severe Acute Respiratory Syndrome (SARS) outbreak, which was declared contained by the World Health Organisation in July 2003;
- MERS-CoV. This is the virus that is responsible for Middle East Respiratory Syndrome (MERS). This virus still exists, but is mostly confined to the Middle East as human-to-human transmission of the virus is rare. The majority of MERS cases are caused by eating or engaging in close contact with camels;
- SARS-CoV-2. This is the full name of the virus that causes COVID-19.
COVID-19 stands for “COronaVIrusDisease-2019“. The number “19” is a reference to the date of the first case in humans, which was recorded in 2019. Some early medical journal reports refer to COVID-19 as “nCoV”, which stands for “novel CoronaVirus”.
Where exactly did COVID-19 come from?
Scientists don’t know for certain. Some believe it came originally from bats: a study conducted in February 2020 found a bat coronavirus that was 96% identical to COVID-19. SARS-CoV – the virus that was responsible for SARS in 2003 – is also thought to have come from bats.
Although the virus may originate in bats, it’s possible it reached humans via another species. This species would have caught the infection from bats before passing it on to humans. In the case of COVID-19, it’s thought this intermediate species may be snakes or pangolins.
It is easiest for viruses to jump between species when multiple species are reared in close proximity. This is why so many viruses and emerging diseases originate from geographical regions where there are markets selling animals for meat that have been held in close proximity to animals of other species. According to the New England Journal of Medicine, over half (55%) of all COVID-19 patients recorded before January 1st 2020 were linked to the Hunan Seafood Wholesale Market in Wuhan, which was a cross-species food market, so it is thought that this cross-species market may have played a role in COVID-19’s transition to humans.
The majority of Chinese or East Asian people do not eat exotic meats or natural wildlife. The existence of “wet markets” (that’s the term normally used in medical literature to denote mostly open-air markets in East Asia, some of which contain wildlife) in China may, however, have played a role in the emergence of COVID-19. Similar problems have arisen in other regions, such as Africa, where bushmeat (wild animals killed for consumption) is a large, and often necessary, part of the human diet. It is thought HIV was transmitted to humans originally through the consumption of bushmeat, primarily that of non-human primates.
One of the major questions raised by this pandemic is what impact COVID-19 might have on the trade and consumption of wildlife. Vox has produced a detailed explainer video on this topic that’s worth a watch:
At the beginning of the COVID-19 outbreak, the Chinese government banned the consumption and farming of wild animals, but wild animals were still permitted for use in traditional Chinese medicine. On April 13th, 2020, the Chinese authorities re-opened wet markets in Wuhan.
Why has this virus spread between humans so easily?
We don’t yet know. But there’s increasing evidence that both pre- and asymptomatic cases are responsible for a high proportion of the COVID-19 spread. This wasn’t true for SARS or MERS.
What are the symptoms of COVID-19 and how does it harm you?
The symptoms vary massively, but to watch out for are a fever, dry cough and shortness of breath. Consult your local official public health body for more complete information: click here for NHS guidance.
Some COVID-19 patients primarily experience gastrointestinal symptoms – vomiting, loss of appetite, diarrhoea and abdominal pain – which has been under-reported in the mainstream press. One study published in the American Journal of Gastroenterology in March found that around 50% of COVID-19 sufferers in Wuhan had at least one gastrointestinal symptom. One ER doctor in New York commented in a recent documentary that healthcare workers had been underprepared for COVID-19 patients who presented only with gastrointestinal symptoms. You can watch her report here:
If COVID-19 makes you ill enough you need to visit a hospital, this will likely be because of breathing problems and pneumonia. 20% of known COVID-19 sufferers, on average, suffer from pneumonia or breathing problems that lead to their hospitalisation. Pneumonia happens when the small air sacs in the lungs, called alveoli, become inflamed. Pneumonia can vary from mild to severe. Most fatalities, however, occur when a COVID-19 patient with pneumonia goes on to suffer from ARDS, or Acute Respiratory Distress Syndrome. ARDS occurs when the lungs suffer from severe inflammation, which is caused by the body’s immune system attacking healthy lung cells in an attempt to fight infection. ARDS severely limits the body’s ability to exchange oxygen for carbon dioxide, and even those who survive ARDS will likely experience lung damage. The only treatment for ARDS is to place sufferers on artificial respirators that try to breathe for them while their lungs can’t.
If you recover from COVID-19, are you immune?
The fair answer is that we actually don’t know. Antibodies to COVID-19 have been detected in some who have recovered from the virus, which might be an early sign that survivors have some degree of immunity, but we don’t know if this happens to all survivors or how long the immunity lasts. There have been examples of COVID-19 cases that have been discharged from hospitals only to reacquire symptoms a week later. We do not yet know whether this is caused by a second infection or some kind of reactivation of the first.
There are also questions regarding lung damage of those who suffer from COVID-19. CT scans of hospitalised COVID-19 patients have shown bilateral ground glass opacities, which indicate a filling of air spaces in the lungs of fluid. SARS had a similar effect on people’s lungs.
Are there any treatments for COVID-19?
There are no known medications you can take for COVID-19. The aim of hospitalisation is to keep sufferers alive long enough for the immune system to fight off the virus – treatments in hospital are supportive and mostly involve trying to improve the amount of oxygen entering the body while the lungs are not fully functional. Even those who recover from ARDS, the stage of COVID-19 infection that is most likely to kill you, will likely suffer lung damage.
The World Health Organisation is conducting multi-country clinical trials of four potential COVID-19 treatments. These trials are unusual in that they do not involve a control group: clinical trials normally treat one group of sufferers with a proposed medicine and another (called the “control group”) with something that looks identical to the medicine but has no physical effect on the sufferer. This is normally done to try and prevent the psychology of the trial participants, often referred to as “the placebo effect”, altering the results of the trial. The World Health Organisation has removed these usual protocols in an attempt to find a treatment for COVID-19 as rapidly as possible. The trials are being conducted across 70 countries and more information can be found here.
The United States is also conducting a trial into the use of blood plasma from those who have recovered from COVID-19, which will likely contain antibodies to the virus, on those with severe COVID-19 symptoms.
A number of clinical trials are taking place across several countries in an attempt to find a safe and effective vaccine for COVID-19. The usual animal testing has been bypassed in an attempt to source a vaccine as quickly as possible. Even without this usual safety protocol, it will usually take 18+ months to develop a vaccine – and any of the vaccines currently in development may fail at the clinical trial stage. Attempts to find a safe and effective vaccine for SARS and MERS failed.
How Can I Help Fight COVID-19?
The answer’s simple: listen to and follow official public health advice, wash your hands and practice social distancing, don’t spread fake news about the virus and – most importantly – stay at home.